Candida auris infections, a global public health concern in recent years, pose a significant risk in healthcare settings, especially for individuals with underlying medical conditions. Researchers suggest that climate change may be responsible for the sudden emergence of this fungus, which was not previously found in humans before 2009. These fungal infections can lead to severe illnesses, including bloodstream, wound, and respiratory infections, with mortality rates ranging from 30% to 60%.
In 2016, hospitals in New York first identified this rare and dangerous infection, which had never been seen in the United States. Following this discovery, research laboratories reviewed past specimens and found traces of the fungus dating back to at least 2013. Since then, New York City has become a hotspot for Candida auris infections, consistently recording the highest number of cases in the country. Although the illness has spread to other areas, New York state remains a major center for these infections, according to data from the Centers for Disease Control and Prevention (CDC).
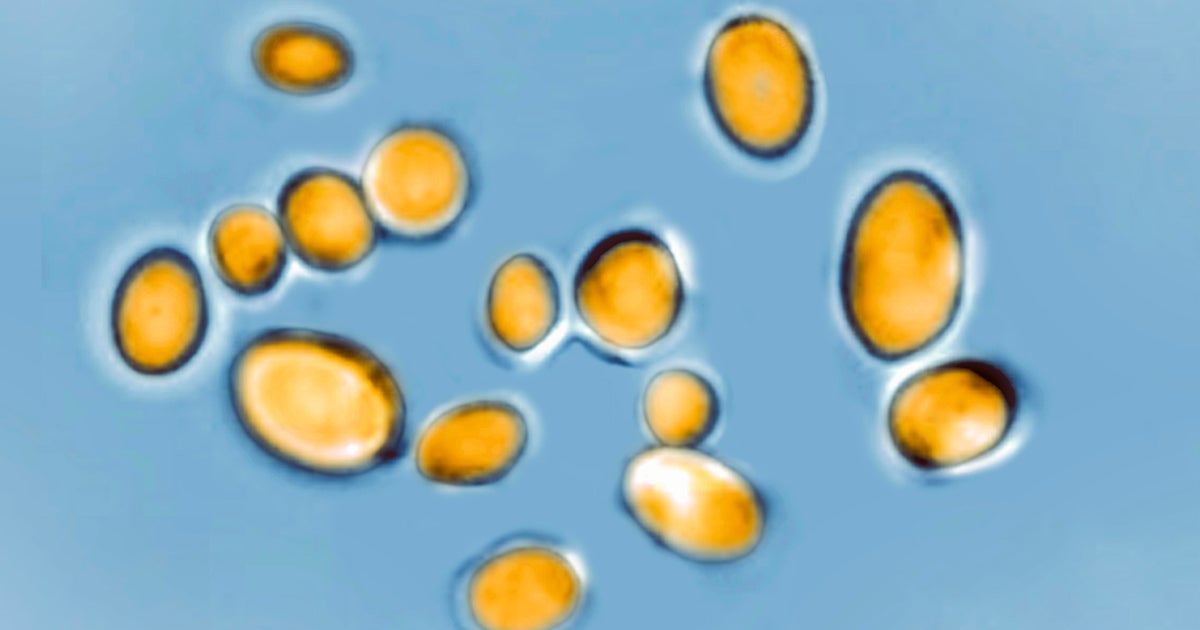
While Nevada and California had the most cases last year, clinical identification of Candida auris was reported in patients from 29 states across the US. The fungus is resistant to most antifungal drugs, making it a major concern for healthcare professionals. Candida auris, a yeast visible under an optical microscope, has caused numerous deaths worldwide. It primarily affects individuals in hospital and nursing home settings.
Historically, humans and other mammals have been protected from many fungal pathogens due to their warmer body temperatures. However, rising temperatures associated with climate change can lead to the adaptation of fungi to higher temperatures, potentially compromising human resistance. This may explain the emergence of Candida auris, which spontaneously appeared in different climates like Venezuela, India, and South Africa. Researchers suggest that as the world continues to warm, certain fungal pathogens may overcome the “temperature barrier” imposed by warm-blooded mammals.
Initially, Candida auris cases were linked to individuals who had traveled to the US from other regions. However, most cases now occur locally, primarily spreading within healthcare settings. The number of clinical cases in the US has dramatically increased by over 1,200% since 2017, reaching 2,377 confirmed cases last year. Europe has also witnessed a surge in cases, with numbers almost doubling from 2020 to 2021.
The severity of Candida auris infections, combined with its resistance to traditional antifungal treatments, makes it a nightmare scenario for infectious disease experts. The fungus is typically resistant to the most common antifungal medication and may also resist another drug used for severe catheter fungal infections. Consequently, healthcare professionals struggle to find effective treatments for patients, putting their lives at risk.
Scientists, academics, and public health organizations are actively studying the emergence of Candida auris. The prevailing theory for its origin is climate change. Additionally, the fungus might have always existed in the human body without causing infection, but recent changes in the environment and human activities may have triggered its pathogenic behavior. Understanding the origin and mechanisms of Candida auris is crucial because it poses a significant threat to human health.
Diagnosing Candida auris is challenging, as its symptoms are nonspecific and may be attributed to various causes. Sepsis, fever, and low blood pressure are common symptoms of infection, but they can result from different illnesses. Currently, a blood test is the most common diagnostic method, although it may miss approximately half of the cases. Newer technologies are emerging to improve detection but are costly and not widely available.
In addition to the increasing number of cases, popular culture has played a role in raising awareness of fungal infections. For example, the HBO series “The Last of Us” depicts a fictional world affected by a fungal outbreak. While the concept of fungi transforming humans into zombies is fictional, addressing climate change and its impact on the spread of diseases is an urgent real-world challenge.
According to experts, climate change exerts selection pressure on microbes by creating more hot days. Each day with high temperatures provides a selection event for microbes, increasing the likelihood of adaptation and survival. Fungal infections were not previously a major concern in the field of mycology, but with the changing climate, they are now a pressing issue.
In conclusion, Candida auris infections have emerged as a global public health threat, especially in healthcare settings. The rise of this fungus may be attributed to climate change, which impacts fungal pathogens’ ability to adapt. Hospitals in New York state initially identified the infection, which has since become widespread across the US and internationally. Candida auris poses challenges in diagnosis and treatment, leading to high mortality rates amongst affected individuals. As the world grapples with the impact of climate change, addressing the spread of fungal infections becomes a critical task to protect public health.
Denial of responsibility! VigourTimes is an automatic aggregator of Global media. In each content, the hyperlink to the primary source is specified. All trademarks belong to their rightful owners, and all materials to their authors. For any complaint, please reach us at – [email protected]. We will take necessary action within 24 hours.